Introduction
Insulin resistance syndrome is a silent epidemic that affects a staggering 26% to 30% of the global population. We understand that many remain unaware of its implications, and that can be concerning. This condition not only disrupts the body’s ability to manage blood sugar but also opens the door to serious health risks, including type 2 diabetes and cardiovascular diseases.
As you navigate the complexities of this syndrome, you might be wondering: what proactive steps can you take to recognize, manage, and ultimately overcome insulin resistance? You’re not alone in this journey. This article delves into the symptoms, causes, and effective strategies for mastering insulin resistance syndrome. We aim to offer valuable insights that can help you reclaim your health and well-being.
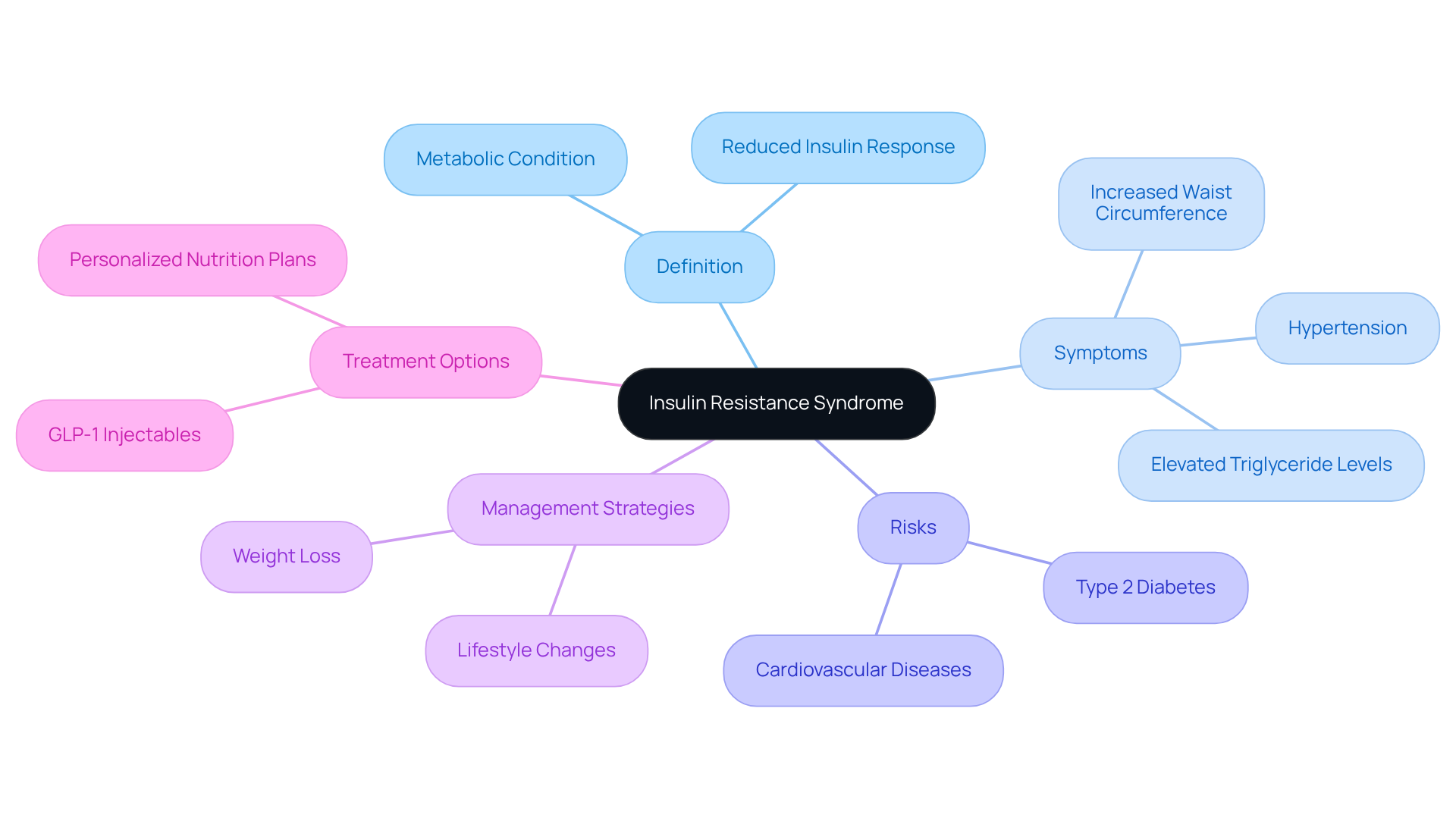
Define Insulin Resistance Syndrome and Its Importance
Insulin resistance syndrome is a metabolic condition that many people face, characterized by the body’s reduced ability to respond to a hormone essential for regulating blood sugar. This syndrome often comes hand-in-hand with a range of metabolic issues, such as obesity, hypertension, and dyslipidemia. Recognizing insulin resistance syndrome is vital, as it significantly increases the risk of developing type 2 diabetes and cardiovascular diseases. Did you know that the global prevalence of insulin resistance is estimated to be between 26% and 30%? This statistic highlights just how widespread this issue is and its impact on public health.
Symptoms of IRS can include:
- Increased waist circumference
- Hypertension
- Elevated triglyceride levels
These factors collectively raise the risk of serious health complications. For instance, individuals with a higher triglyceride-glucose (TyG) index face a greater likelihood of adverse events related to heart failure. Studies show that those in the highest TyG index group have a hazard ratio of 2.15, which is concerning.
Effectively managing insulin resistance syndrome often involves making some lifestyle changes, such as adjusting your diet and increasing physical activity. Research indicates that intensive interventions can significantly reduce the onset of type 2 diabetes. In fact, a modest 7% weight loss through these changes can lead to a remarkable 58% reduction in risk. Health experts emphasize that promoting these lifestyle modifications is crucial in addressing blood sugar issues associated with insulin resistance syndrome, as they can help mitigate related health hazards.
At CT Medical Weight Loss & Beyond, we understand the importance of addressing hormone resistance in our weight loss programs. Our approach includes using GLP-1 injectables, like Semaglutide, which enhance the secretion of a hormone that promotes feelings of fullness, aiding in weight control. These injectables have received FDA approval for treating Type 2 diabetes and have shown promising results in clinical trials for weight loss, making them a safe and effective option for many.
Real-world examples of successful management of insulin resistance syndrome underscore the value of a structured approach. Individuals who adhere to comprehensive health plans often report improved glucose sensitivity and overall wellness. This reinforces the importance of early detection and intervention; heightened clinical awareness can lead to better management strategies and improved long-term health for those affected by glucose intolerance. By combining GLP-1 medications with personalized nutrition plans and lifestyle changes, we empower individuals to achieve lasting health results and effectively navigate the challenges posed by glucose intolerance.
Identify Symptoms of Insulin Resistance
Common symptoms of insulin resistance syndrome can be challenging to navigate, and we understand that recognizing them is the first step toward better health. Here are some signs to look out for:
- Increased Hunger: You might find yourself feeling hungrier shortly after meals. This can happen because of insulin resistance syndrome, which prevents insulin from signaling your body effectively, leaving your blood sugar levels unregulated.
- Fatigue: Persistent tiredness is something many people experience. It can be frustrating when your body struggles to use glucose for energy, leading to exhaustion even after a good night’s sleep.
- Weight Gain: If you notice weight gain, particularly around your abdomen, it’s important to pay attention. The presence of insulin resistance syndrome encourages fat storage in this area, which can be a significant indicator of metabolic issues.
- Skin Changes: You may see dark patches of skin, known as acanthosis nigricans, appearing in places like your neck and armpits. This can signal increased hormone levels in your body.
- Frequent urination and increased thirst can indicate elevated blood sugar levels, which are often linked to insulin resistance syndrome, a condition characterized by reduced sensitivity to hormones that help regulate glucose.
Recognizing these symptoms early is crucial. It allows for timely intervention and management strategies that can make a real difference in your health. Recent findings from endocrinologists highlight that addressing these symptoms can significantly improve health outcomes, especially for those dealing with fatigue and increased appetite, which are common among individuals with insulin resistance syndrome.
You’re not alone in this journey. Many patients have successfully identified these symptoms and sought medical advice, leading to effective management and positive lifestyle changes. Remember, taking action now can pave the way for a healthier future.

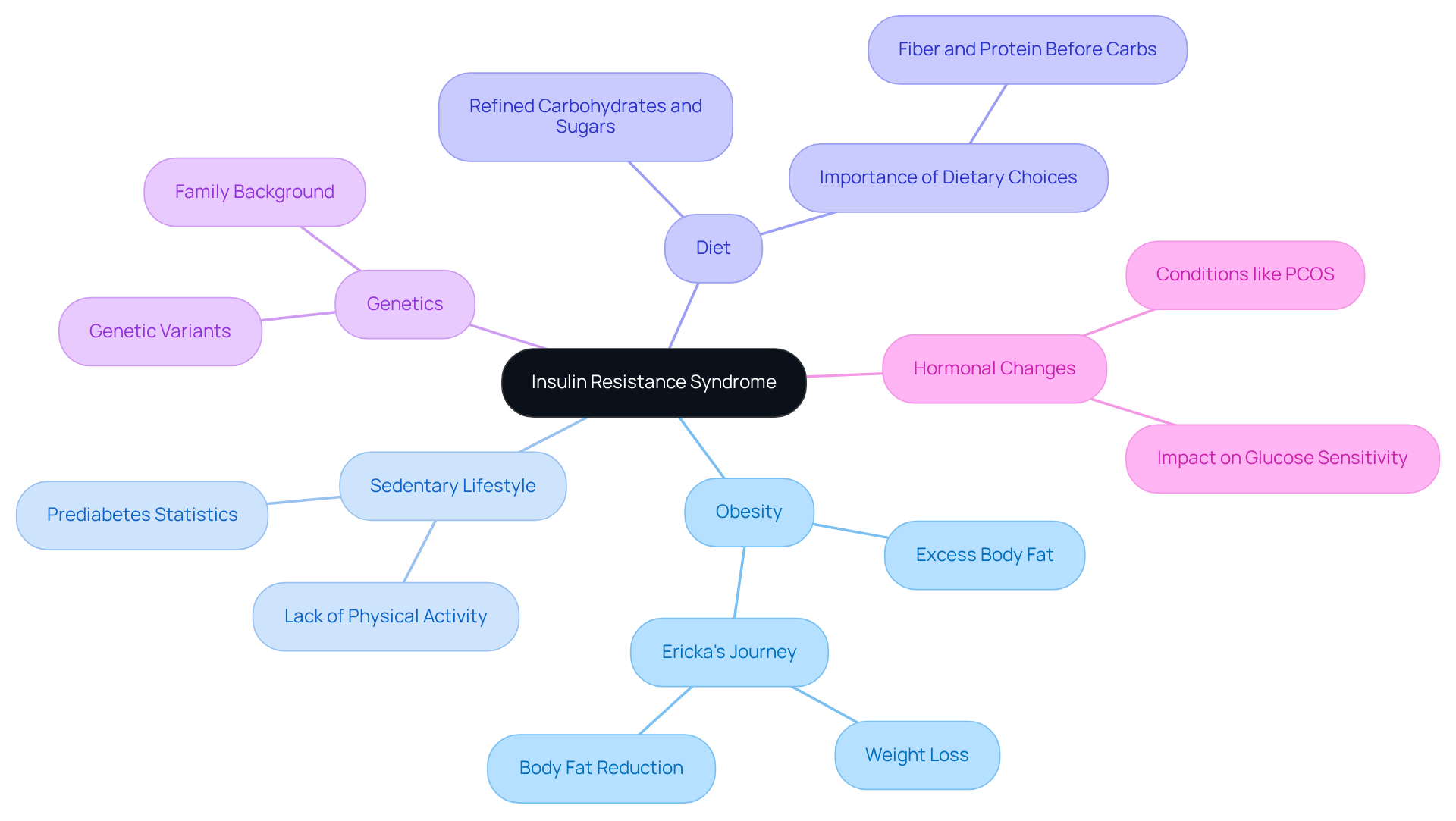
Examine Causes of Insulin Resistance
Understanding insulin resistance syndrome, which refers to the body’s impaired ability to respond to insulin, can be overwhelming, but you’re not alone in this journey. Several factors contribute to insulin resistance syndrome, and recognizing these factors is the first step toward improvement. Here are some key contributors:
-
Obesity: Excess body fat, particularly visceral fat, plays a significant role in developing insulin resistance. Research shows that central fat stores are more closely linked to resistance and type 2 diabetes than peripheral fat stores. This connection is evident across all ethnic groups and body weights, with the risk for diabetes increasing as body fat rises. Take Ericka’s journey at CT Medical Weight Loss & Beyond, for example. Her personalized nutrition program helped her achieve an impressive 18 lbs weight loss and a reduction in body fat percentage from 31% to 22.8%.
-
Sedentary Lifestyle: A lack of physical activity can significantly impair glucose sensitivity. Did you know that one in three adults in the U.S. has prediabetes? This condition is closely associated with obesity and inactivity, often referred to as insulin resistance syndrome. Incorporating regular physical activity, as part of Ericka’s customized workout strategy, can improve glucose sensitivity and help reduce these risks.
-
Diet: High intake of refined carbohydrates and sugars can worsen blood sugar sensitivity. Nutritionists emphasize the importance of dietary choices; for instance, eating fiber or protein before carbohydrates can lower glucose spikes in healthy individuals. Ericka benefited from a custom nutrition program designed specifically around her body, goals, and lifestyle, equipping her with the tools to make lasting dietary changes.
-
Genetics: Your family background can predispose you to glucose resistance, highlighting the importance of understanding your genetic history in managing health.
-
Hormonal Changes: Conditions like polycystic ovary syndrome (PCOS) can interfere with glucose sensitivity, complicating weight management and metabolic health.
By identifying these factors, you can focus on specific areas for enhancement, creating opportunities for effective methods to improve glucose sensitivity and combat insulin resistance syndrome, thereby enhancing overall well-being. Remember, Ericka’s real-time transformation journey is a testament to the power of personalized support and expert coaching in overcoming these challenges. Together, we can navigate this path toward better health.
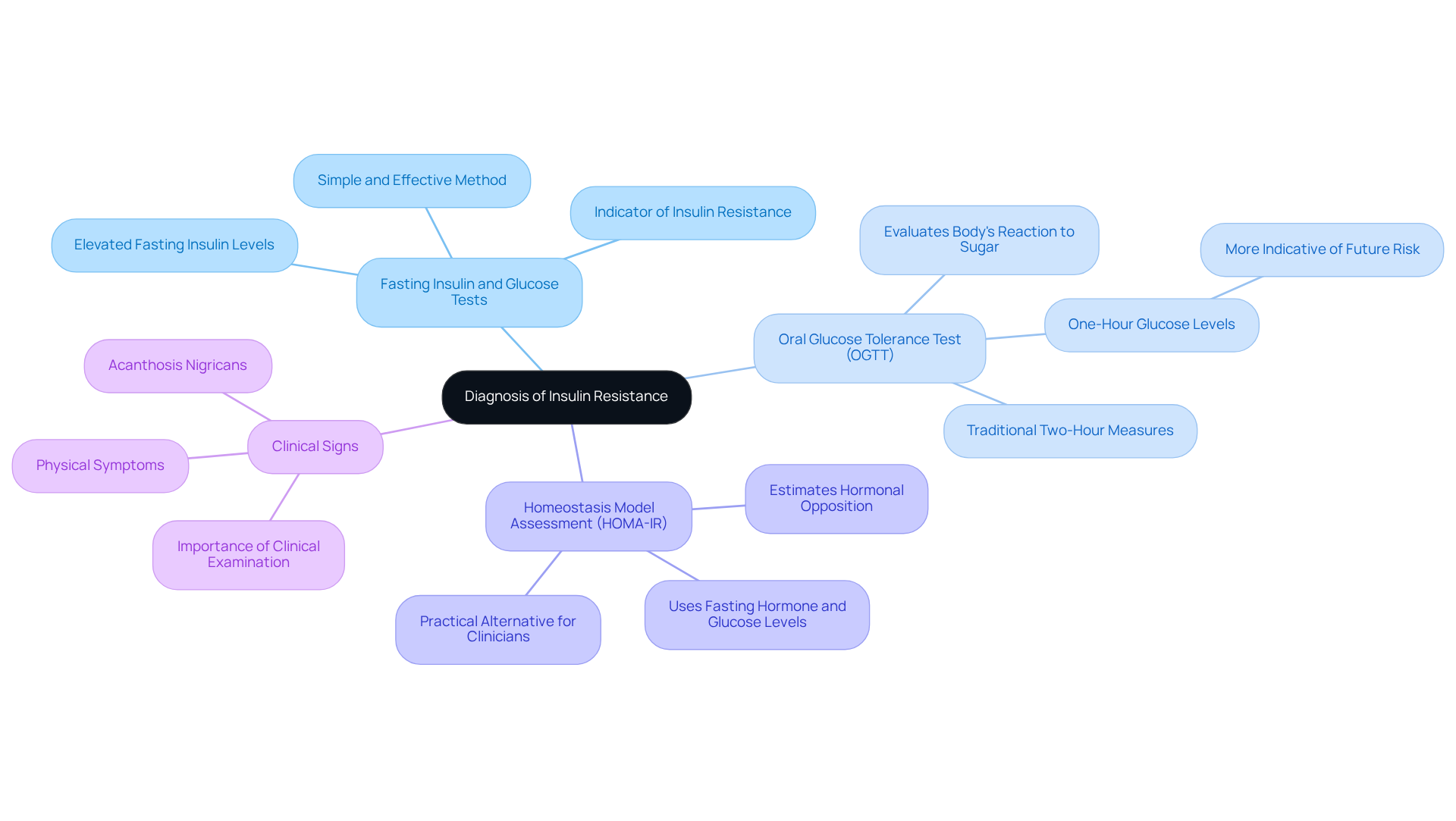
Outline the Diagnosis of Insulin Resistance
Identifying glucose intolerance can feel overwhelming, but it’s important to know that a multifaceted strategy can help. By combining clinical assessments with lab examinations, we can better understand this condition. Here are some key diagnostic methods:
- Fasting Insulin and Glucose Tests: If you find elevated fasting insulin levels, especially when paired with high glucose, it’s a strong indicator of insulin resistance. This method is popular because it’s simple and effective.
- Oral Glucose Tolerance Test (OGTT): This test evaluates how your body reacts to sugar over a specific duration. It offers valuable insights into how effectively your hormone is functioning. Recent studies suggest that one-hour glucose levels during the OGTT might be more indicative of future risk than the traditional two-hour measures.
- Homeostasis Model Assessment (HOMA-IR): This calculation uses fasting hormone and glucose levels to estimate hormonal opposition, providing a practical alternative for clinicians.
- Clinical Signs: Physical symptoms, like acanthosis nigricans, can also assist in diagnosis, underscoring the importance of a thorough clinical examination.
Prompt identification of issues related to insulin resistance syndrome is essential. It allows for timely lifestyle changes that can significantly lower the likelihood of developing type 2 sugar-related illnesses. Research shows that even a modest 7% weight reduction can decrease the onset of type 2 conditions by 58%. This highlights the importance of early intervention.
Moreover, the occurrence of glucose intolerance is concerning, with roughly 22% of U.S. adults over 20 years old affected, and figures rising to 40% among younger individuals. You’re not alone in this journey, and these statistics emphasize the need for proactive screening and diagnosis to combat this growing health issue. We understand that taking the first step can be daunting, but together, we can work towards a healthier future.
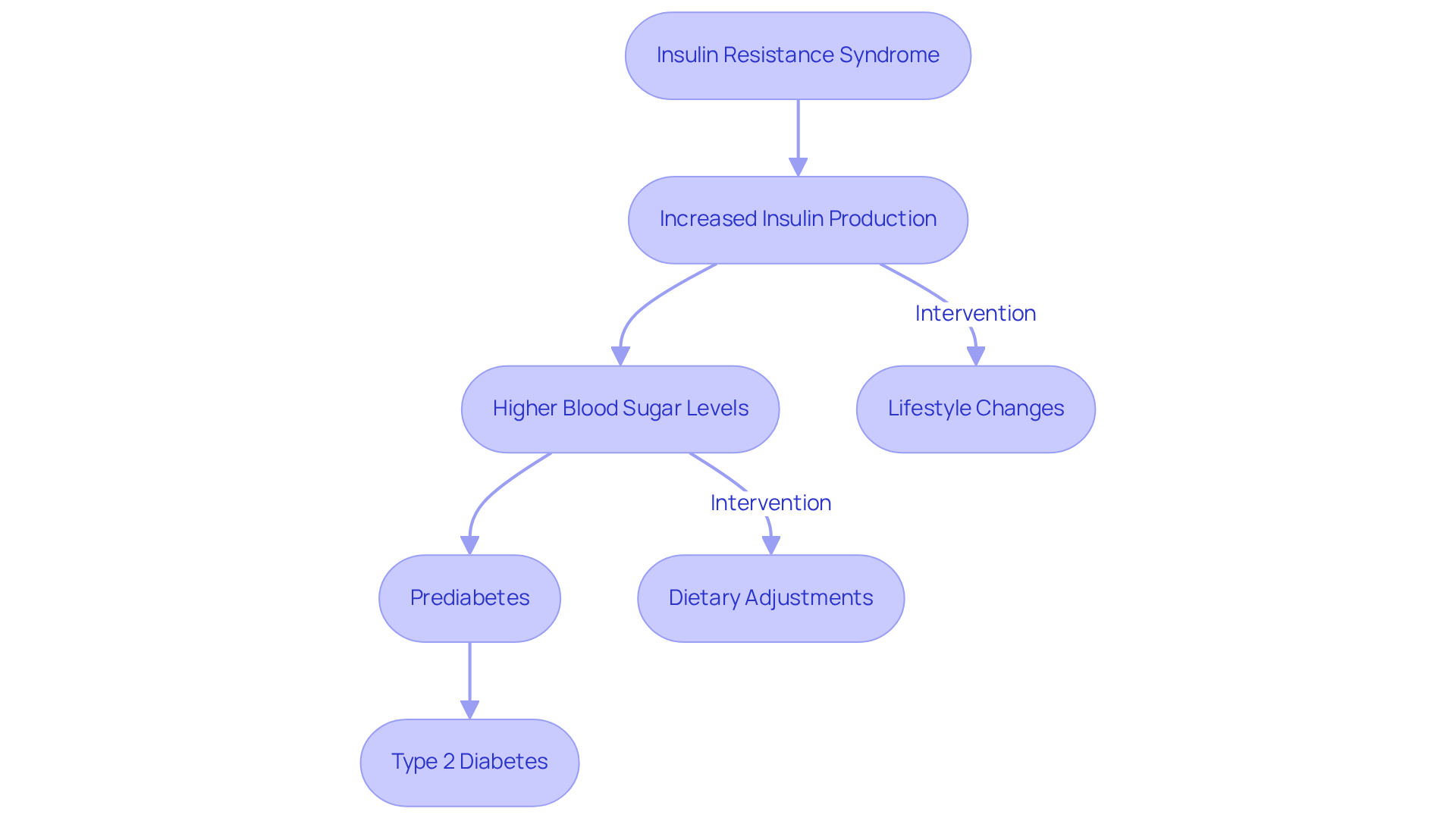
Discuss Progression to Type 2 Diabetes
Insulin resistance syndrome can be a challenging precursor to type 2 diabetes, often developing slowly over several years. We understand that when the body starts developing insulin resistance syndrome, it can feel overwhelming. Initially, the pancreas compensates by producing more insulin, but over time, this mechanism may struggle, leading to higher blood sugar levels. If left unaddressed, this can progress to insulin resistance syndrome, prediabetes, and eventually type 2 diabetes, marked by ongoing high blood sugar.
This progression underscores the importance of early intervention. Experts like Andrew M. Freeman emphasize that lifestyle changes should be the main focus when addressing insulin resistance syndrome. You’re not alone in this journey; many people face similar challenges. In fact, studies show that over 90% of individuals with diabetes have type 2, highlighting the urgent need for effective prevention strategies.
Adopting a high-fiber, microbiome-friendly diet can significantly improve glucose sensitivity. This shows that dietary changes can truly make a difference in reducing health risks associated with diabetes. Moreover, the International Diabetes Federation predicts that by 2050, 1 in 8 adults will be living with diabetes, reinforcing the need for proactive measures.
Taking a structured approach to tackle glucose intolerance-one that includes physical activity and dietary adjustments-can greatly lower the risk of developing type 2 diabetes and its complications, such as serious heart issues, as Freeman points out. A collaborative team strategy is also essential in effectively managing blood sugar challenges, ensuring comprehensive care for those at risk. Remember, you have the power to make positive changes, and support is available every step of the way.
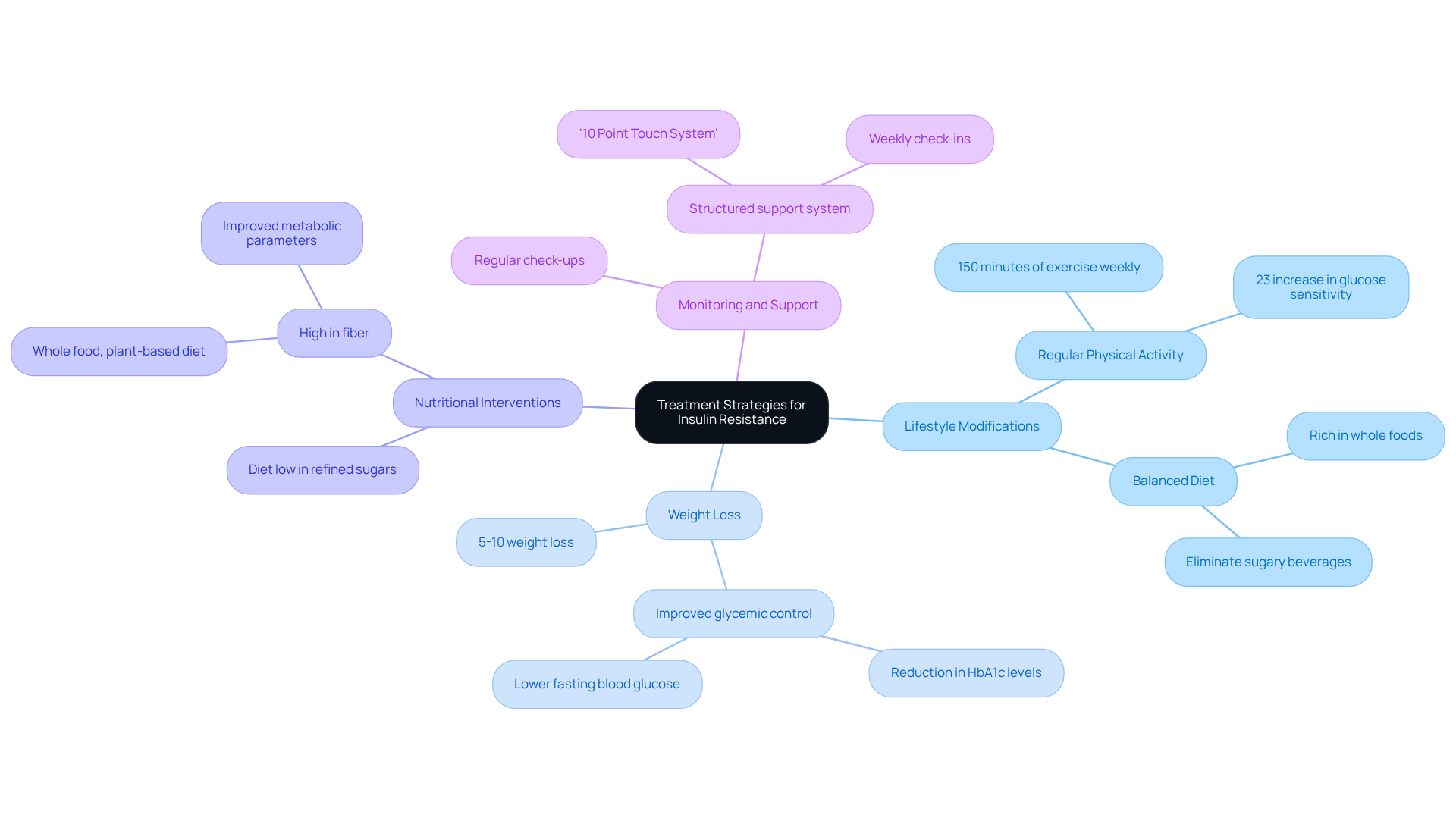
Explore Treatment Strategies for Insulin Resistance
Effective treatment strategies for insulin resistance encompass several key approaches that can truly make a difference in your journey toward better health:
-
Lifestyle Modifications: We understand that making changes can be challenging, but regular physical activity and a balanced diet rich in whole foods are crucial for enhancing insulin sensitivity. Engaging in at least 150 minutes of moderate exercise weekly can lead to significant improvements in metabolic health. For instance, a study showed that participants who followed a structured routine change program experienced a 23% increase in glucose sensitivity, highlighting the positive impact of regular physical activity. At CT Medical Weight Loss & Beyond, we offer tailored app-based exercise programs designed to fit your personal routine, ensuring you can sustain your activity levels effectively.
-
Weight Loss: You’re not alone in this journey. Attaining even a slight weight decrease of 5-10% can significantly improve glucose sensitivity. Research indicates that individuals with type 2 diabetes who lost weight through behavioral changes saw remarkable improvements in glycemic control, with reductions in HbA1c levels and fasting blood glucose. This underscores the importance of weight management in addressing blood sugar resistance. Our transformative 16-week weight loss program at CT Medical Weight Loss & Beyond is crafted to help you lose up to 25 lbs while embracing a healthier lifestyle.
-
Nutritional Interventions: Managing blood sugar levels is essential, and a diet low in refined sugars and high in fiber can be a game changer. Eliminating sugary beverages and processed foods can lead to better insulin sensitivity. For example, individuals in a modification program who adopted a whole food, plant-based diet reported improved metabolic parameters, including reduced cholesterol levels and better glucose regulation. At CT Medical Weight Loss & Beyond, our personalized custom nutrition program offers tailored support, ensuring you receive a nutrition plan that aligns with your individual goals and daily routines.
-
Monitoring and Support: Regular check-ups and support from healthcare professionals are vital for maintaining behavioral changes. Ongoing encouragement can help you stay focused on your weight loss and nutrition objectives, ultimately leading to lasting improvements in glucose sensitivity. Our structured support system, including the ’10 Point Touch System,’ weekly check-ins, and monthly newsletters, ensures you receive the guidance and accountability you need to succeed.
Integrating these strategies not only helps in addressing glucose intolerance but also promotes a healthier lifestyle overall. Remember, you’re not alone in this journey; we’re here to support you every step of the way.
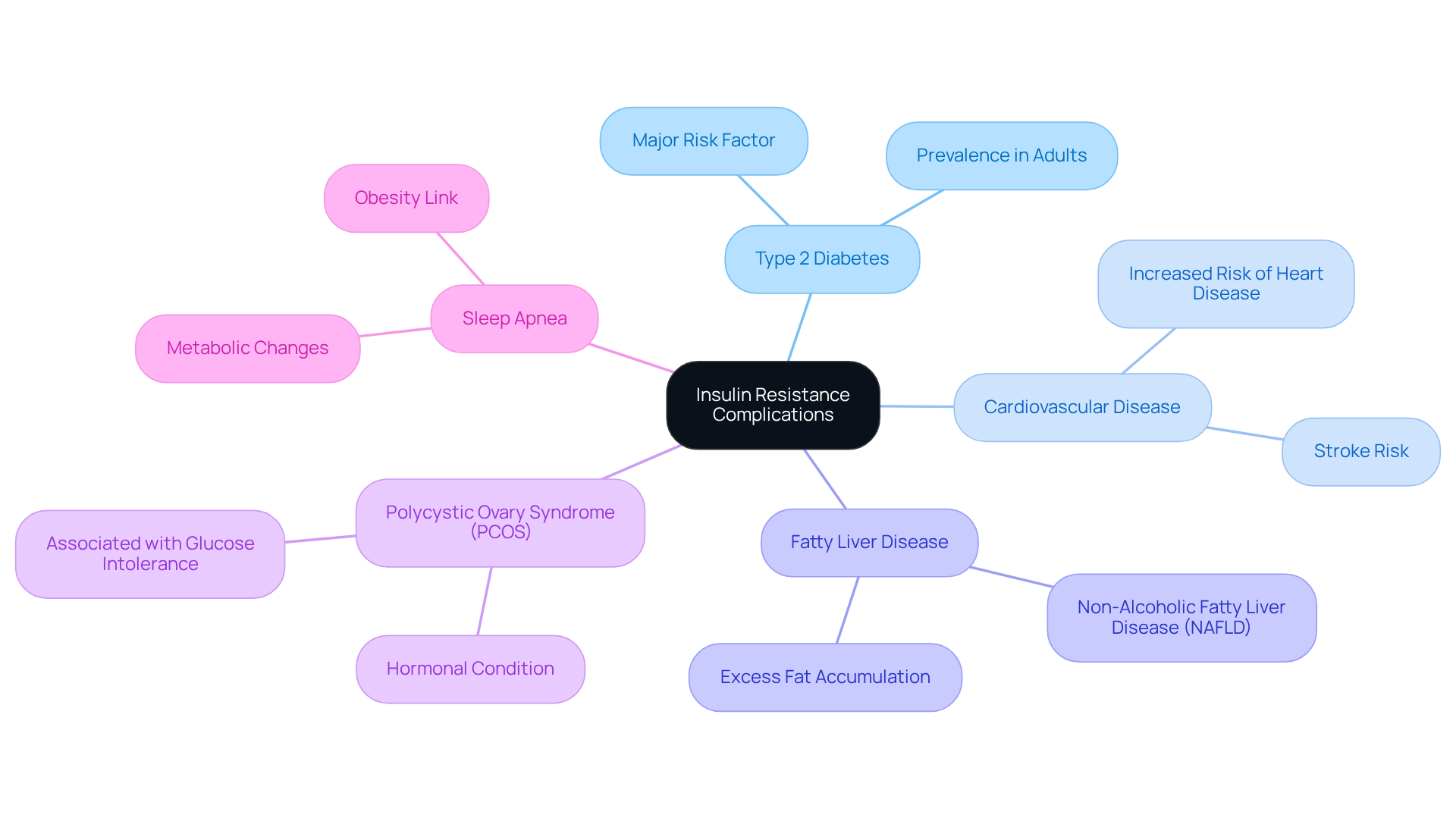
Review Complications of Insulin Resistance
Insulin resistance can lead to several serious health complications that many people face. We understand that navigating these challenges can be overwhelming, but recognizing them is the first step toward better health. Here are some of the complications you might encounter:
- Type 2 diabetes: As we’ve discussed, insulin resistance is a major risk factor.
- Cardiovascular disease: There’s an increased risk of heart disease and stroke, often linked to factors like hypertension and dyslipidemia.
- Fatty liver disease: Excess fat accumulation in the liver can result in non-alcoholic fatty liver disease (NAFLD).
- Polycystic ovary syndrome (PCOS): This hormonal condition is associated with glucose intolerance.
- Sleep apnea: Obesity and metabolic changes can heighten the risk of obstructive sleep apnea.
Recognizing these complications can motivate you to take proactive steps in managing your health. At CT Medical Weight Loss & Beyond, we offer personalized medical weight loss solutions designed to address these complications through innovative treatments and holistic care.
Comprehending the connection between glucose intolerance and insulin resistance syndrome is vital for effective management and achieving lasting outcomes. Remember, you’re not alone in this journey; we’re here to support you every step of the way.
Implement Lifestyle Changes for Effective Management
To effectively manage insulin resistance, we understand that making lifestyle changes can feel overwhelming. However, small steps can lead to significant improvements in your health. Here are some compassionate suggestions to consider:
-
Adopt a balanced diet: Emphasize whole foods, including a variety of vegetables, fruits, whole grains, and lean proteins. A whole food, plant-based diet has been shown to enhance sensitivity to glucose and improve glycemic control. This approach can be a strong ally for those at risk of diabetes, helping you feel more in control of your health.
-
Increase physical activity: Aim for at least 150 minutes of moderate-intensity exercise each week, such as brisk walking or cycling. Regular physical activity not only improves sensitivity to glucose but also supports weight management, which is essential for metabolic health. Remember, even light exercise after meals can help your body manage glucose more effectively, so every little bit counts!
-
Manage stress: Incorporate stress-reducing practices like yoga, meditation, or deep-breathing exercises into your routine. Persistent stress can lead to hormonal imbalances that worsen glucose resistance. By prioritizing stress management, you’re taking an important step toward a healthier lifestyle.
-
Prioritize sleep: Aim for 7-9 hours of quality sleep each night. Sufficient rest is crucial for preserving glucose sensitivity and regulating appetite. Research shows that sleep deprivation can increase cravings for sugary and high-carb foods, complicating diabetes management. You’re not alone in this journey; many people struggle with sleep, but making it a priority can lead to positive changes.
-
Regular monitoring: Keep track of your blood sugar levels and consult with healthcare providers for personalized guidance. Monitoring fasting blood sugar levels can help you understand how your body manages glucose overnight, allowing for better meal and exercise planning.
By making these changes, you can significantly improve your insulin sensitivity and overall health. Remember, every step you take is a step toward a more balanced and sustainable lifestyle. You’re not alone in this journey, and with support and understanding, you can achieve your health goals.
Conclusion
Insulin resistance syndrome is a significant metabolic condition that deserves our attention, given its widespread impact on health. We understand that navigating the complexities of this syndrome can be challenging, but by grasping its definition and importance, you can take meaningful steps toward better health. The alarming prevalence of insulin resistance – between 26% and 30% globally – underscores the urgency for awareness and action.
Throughout this discussion, we’ve uncovered key insights about insulin resistance. Symptoms like increased hunger, fatigue, and weight gain can be concerning, and various causes, including obesity and a sedentary lifestyle, contribute to this condition. Early diagnosis is crucial; methods like fasting insulin tests can help identify the issue before it progresses to type 2 diabetes. This highlights the need for proactive management.
Effective treatment strategies are available, and they include:
- Lifestyle modifications
- Nutritional interventions
- Regular monitoring
These approaches play a vital role in improving insulin sensitivity and overall health. Remember, addressing insulin resistance syndrome isn’t just about managing symptoms; it’s about empowering you to take control of your health.
By adopting a balanced diet, increasing physical activity, and prioritizing your mental well-being, you can achieve significant improvements. We know the journey may seem daunting, but with the right support and resources, you’re not alone in this. Together, we can navigate the challenges of insulin resistance and work toward a healthier future. Taking these proactive steps today can lead to lasting positive outcomes, making it essential to prioritize this aspect of your metabolic health.
Frequently Asked Questions
What is insulin resistance syndrome?
Insulin resistance syndrome is a metabolic condition where the body has a reduced ability to respond to insulin, a hormone essential for regulating blood sugar. It is often associated with metabolic issues like obesity, hypertension, and dyslipidemia.
Why is it important to recognize insulin resistance syndrome?
Recognizing insulin resistance syndrome is crucial because it significantly increases the risk of developing type 2 diabetes and cardiovascular diseases. The global prevalence of insulin resistance is estimated to be between 26% and 30%, highlighting its widespread impact on public health.
What are common symptoms of insulin resistance syndrome?
Common symptoms include increased waist circumference, hypertension, elevated triglyceride levels, increased hunger, fatigue, weight gain (especially around the abdomen), skin changes like dark patches (acanthosis nigricans), frequent urination, and increased thirst.
How does insulin resistance syndrome affect health?
Insulin resistance syndrome raises the risk of serious health complications, including type 2 diabetes and cardiovascular diseases. For example, individuals with a higher triglyceride-glucose (TyG) index have a significantly increased likelihood of adverse heart-related events.
What lifestyle changes can help manage insulin resistance syndrome?
Effective management often involves lifestyle changes such as adjusting diet and increasing physical activity. Research indicates that a modest 7% weight loss can lead to a 58% reduction in the risk of developing type 2 diabetes.
What role do GLP-1 injectables play in managing insulin resistance syndrome?
GLP-1 injectables, like Semaglutide, enhance the secretion of hormones that promote feelings of fullness, aiding in weight control. They have received FDA approval for treating type 2 diabetes and have shown promising results for weight loss.
How can early detection of insulin resistance syndrome improve health outcomes?
Early detection allows for timely intervention and management strategies, leading to better health outcomes. Individuals who follow structured health plans often report improved glucose sensitivity and overall wellness.
What should individuals do if they suspect they have insulin resistance syndrome?
Individuals should recognize the symptoms and seek medical advice for effective management and lifestyle changes, which can lead to a healthier future.




